Background
Chronic Achilles tendinopathy is responsible for a severe reduction in physical performance and persistent pain. There is currently a number of therapeutic options and the local administration of growth factors is an emerging treatment strategy. In particular, platelet-rich plasma (PRP) is a widely used way to provide a local regenerative stimulus for tendon healing. The aim of this study was to document the mid-term results obtained after treating recalcitrant Achilles tendinopathy with injections of high concentrate, leucocyte-rich PRP.
Materials and methods
Twenty-seven patients (mean age: 44.6 years; 22 men and 5 women) affected by chronic mid-portion Achilles tendinopathy (7 bilateral, for a total of 34 tendons), refractory to previous treatments, were enrolled. Patients were treated with three ultrasound-guided intra-tendinous injections of PRP at 2-week intervals. Patients were prospectively evaluated at baseline, and then at 2, 6, and up to a mean of 54.1 months of follow-up (minimum 30 months), using the following tools: Blanzina, VISA-A, EQ-VAS for general health, and Tegner scores.
Results
The VISA-A score showed a significant improvement: the baseline score of 49.9±18.1 increased to 62.9±19.8 at 2 months (p=0.002), with a further improvement at 6 months (84.3±17.1, p<0.0005), and stable results at 4.5 years (90.0±13.9). The EQ-VAS score also showed a similar positive trend. An evaluation of the activity level confirmed these findings, showing a significant improvement in the Tegner score over time (p=0.017 for the final evaluation). The longer duration of symptoms before treatment was associated with a slower return to sport (p=0.041).
Discussion
PRP injections produced good overall results for the treatment of chronic recalcitrant Achilles tendinopathy with a stable outcome up to a medium-term follow-up. Longer symptom duration was related with a more difficult return to sporting activity.
Introduction
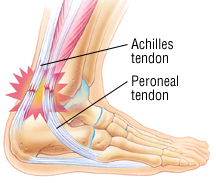
Achilles tendinopathy, in particular pathology of the mid-portion of the tendon, is one of the most common findings in a sport-active population, especially among long-distance runners, and is responsible for a severe reduction in physical performance and persistent pain over several years1,2. Despite being often considered a “sport-related injury”, studies have revealed that this pathology may also affect an older population with less involvement in sporting activities, thus explaining the social impact of Achilles tendinopathy3,4.
The treatment of this condition is a real challenge for orthopaedic surgeons and sports medicine physicians and it is not always possible to achieve a good outcome. A number of options5–7 are available, ranging from rehabilitation protocols to injective treatment and surgery. Among these, the local administration of growth factors is an emerging treatment strategy which aims at providing a regenerative stimulus in a tissue, the tendon, characterised by a poor healing ability8. In particular, platelet-derived growth factors are the most widely used way to provide a local regenerative stimulus for tendon healing9,10. Platelet granules are rich in important molecules involved in the process of responding to damage and might be beneficial in conditions characterised by chronic, degenerative processes11–15. Platelet-rich plasma (PRP) has been used to a variable degree in recent years in the field of musculoskeletal pathologies16 and, in part as a consequence of the use of ultrasonography for selective intra-lesion administration, it has become especially common in the management of tendinopathy. Despite its widespread use for the treatment of Achilles tendinopathy, only a few studies have described the clinical outcome after injection treatment with PRP, and most of them were of poor methodological quality. Up to now only one randomised controlled trial has compared the effectiveness of a single PRP injection against saline solution for the management of Achilles tendinopathy in 54 patients17,18. The authors of this study reported an improvement in both groups of patients, without statistical difference in terms of clinical results between patients treated with PRP or saline, both at 6 and 12 months of follow-up. Although these findings might discourage clinicians from using PRP to treat Achilles tendinopathy, there are some important limitations in the study design that need to be taken into account before sentencing the ineffectiveness of PRP. First of all it should be taken into consideration that, in the case of saline injections, needling itself might be a treatment, involving mechanical stimulation and bleeding of the degenerated tendon tissue, and therefore the good results reported after saline injections cannot be ascribed only to a placebo effect. Furthermore, the mean age of the patients in the study was notably higher than that of the usual sport-active population, which is normally treated with this regenerative approach; older subjects might be less responsive to the biological effects of PRP. Another point to consider is that a single injection of PRP was administered, whereas other authors have preferred to use repeated PRP injections to guarantee a better and long-lasting action of the platelet-derived growth factors. Another, potentially major, weakness of the study is that the PRP was not activated; the researchers relied on in situ activation provided by the contact of the PRP with autologous collagen. This choice might be questioned because platelet gel formation is delayed and tendon contraction might squeeze the liquid PRP away from the injection site. Self-activation might, therefore, be too slow or insufficient to guarantee the local release of adequate amounts of growth factors. In view of these remarks, and also considering the positive clinical results documented in other trials, this study represents an important landmark in the field, but the question about the real role of PRP in the management of Achilles tendinopathy still remains open and worthy of further investigation.
Another key aspect to consider is that there are several different PRP formulations, which differ in terms of cell type content, platelet concentration, storage modalities, activation methods and protocols for therapeutic application19. If a particular type of PRP has proven to be less effective in treating Achilles tendinopathy, it does not exclude other PRP formulations from being more suitable and beneficial for this particular pathology. In fact, the goal of current research is to establish whether there are some particular characteristics of PRP and some specific features of tendon lesions that might represent clear indications for safe, effective use of PRP in tendinopathy. For this purpose it is essential to provide data about different PRP formulations used to treat Achilles tendinopathy, especially in the case of long-term studies, since such data might demonstrate not only the safety and possible efficacy of PRP, but also the stability of the clinical outcome.
The aim of this study was, therefore, to evaluate the therapeutic effects of repeated injections of laboratory-made, high-concentrate, leucocyte-rich PRP, administered to promote the healing of chronic, recalcitrant Achilles tendinopathy, documenting the quality and duration of clinical improvement in a large cohort of patients up to a mid-term follow-up.
Conclusions
Repeated intra-tendinous injections of autologous PRP produced good results in the treatment of chronic recalcitrant Achilles tendinopathy, with a stable clinical improvement maintained up to a mid-term follow-up. Longer duration of symptoms and lower pre-treatment functional level were responsible for a more difficult return to sporting activities.
For the entire study, please click on the link below:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4212034/